We’re Your Community for Suicide-Specific Care.
The people behind CAMS-care are suicidology experts committed to enhancing our systems of care and saving lives. We’re here to support you navigate suicide prevention and treatment with empathy, compassion, and evidence-based solutions.
Leadership

Colleen Kelly, Esq.
Founder & Legal Counsel

Andrew Evans
President & COO

Kevin Crowley, Ph.D.
Training Solutions – U.S.

Mariam Gregorian, Ph.D.
Training Solutions – U.S.

Anne Wiemers
Director of Operations

Tanisha Jarvis
Diversity Consultant

Ashleigh Edelman
Website Marketing Director

Tracy Kelly
Director of Marketing Strategy

Heidi Hamamoto
Operations Systems Manager

Rachel Bryer
Billing & Fulfillment Manager

Catherine Gorzynski
Customer Success Manager

Meghan Zavadil
Operations Specialist
Our Consultants

Jennifer Crumlish, Ph.D., ABPP
Consultant
Clinical Psychologist and Assistant Director, The Catholic University of America Suicide Prevention Laboratory, Washington, DC.

Mariam Gregorian, Ph.D.
Consultant
Clinical Psychologist, Private Practice, Washington, D.C.

Kevin Crowley, Ph.D.
Consultant
Clinical Psychologist, Capital Institute for Cognitive Therapy, Washington, D.C.

Melinda Moore, Ph.D.
Consultant
Clinical Psychologist and Associate Professor of Psychology, Eastern Kentucky University, Richmond, KY.

Natalie Burns-Iaquinto, LMSW, MA
Consultant
Licensed Master Social Worker, Catholic University
Senior Clinical Social Worker, University of Michigan Medicine

Amy Brausch, Ph.D.
Consultant
Clinical Psychologist and Associate Professor of Psychological Sciences, Western Kentucky University, Bowling Green, KY.

Raymond P. Tucker, Ph.D.
Consultant
Assistant Professor of Psychology, Louisiana State University (LSU)
Clinical Assistant Professor of Psychiatry, Louisiana State University Health Sciences Center (LSUHSC)/Our Lady of the Lake (OLOL)

Kurt D. Michael, Ph.D.
Consultant
Clinical Child and Adolescent Psychologist, Aeschleman Distinguished Professor, Appalachian State University (Retired), Senior Clinical Director, Jed Foundation, High School Programs

Samantha Chalker, Ph.D.
Consultant
Clinical Psychologist, San Diego, CA
Clinical Psychologist, Assistant Professor, Department of Psychiatry, University of California, San Diego, Research Scientist, VA San Diego Healthcare System

Blaire Ehret, Ph.D.
Consultant
Clinical Psychologist, Assistant Program Manager and Clinical Supervisor, Psychosocial Rehabilitation and Recovery Center, VA San Diego Healthcare System, Assistant Professor, Department of Psychiatry, University of California, San Diego, Board Member, Survivors of Suicide Loss, San Diego

John Drozd, Ph.D., ABMP
Consultant
Clinical Psychologist, Board Certified Medical Psychologist, Academy of Medical Psychology

Josephine Au, Ph.D.
Consultant
Assistant Clinical Professor/Associate Director of Clinical Training, Department of Applied Psychology, Northeastern University, Psychologist/Lecturer, McLean Hospital/Harvard Medical School

Asher Siegelman, Ph.D.
Consultant
Clinical Psychologist, PsychCare of Maryland
Beit Shemesh, Israel
CAMS-care Israel

Emma Cardeli, Ph.D.
Consultant
Clinical and Research Psychologist
Department of Psychiatry and Behavioral Sciences
Boston Children’s Hospital/Harvard Medical School

Zaffer Iqbal, Ph.D., DClinPsy, AFBPsS
Consultant
Head of Psychological Services and Consultant Clinical Psychologist, Navigo CiC (NHS) UK; Professor, Faculty of Health Sciences, University of Hull, UK

Paulina Arenas-Landgrave, Ph.D.
Consultant
Clinical Psychologist and Full Professor of Psychology, National Autonomous University of Mexico, Mexico City.

Sarah Thompson, BA, MSc, Dclin Psych
Consultant
Senior Clinical Psychologist, Accredited Schema Therapist and private practitioner

Remco (R.F.P.) de Winter, MD Ph.D.
Consultant
Psychiatrist and chairman of the medical directorate of mental health institution Rivierduinen, senior researcher at the Free University (VU, Amsterdam), Faculty of Clinical Psychology and the Parnassia Academy, lecturer at the RINO Amsterdam.
Are you interested in becoming a CAMS-care Consultant?
We’d love to connect with you!
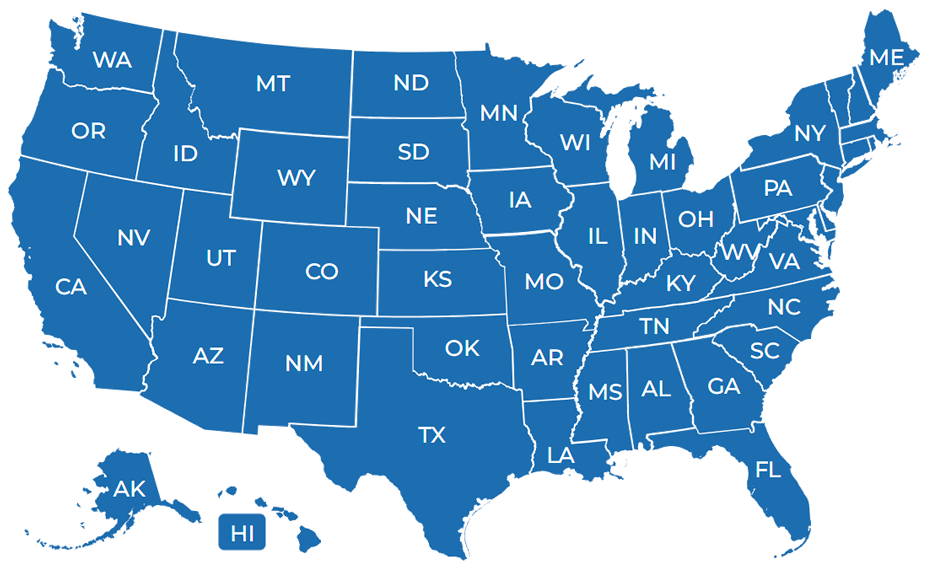
Clinician Locator
Find a CAMS-Trained™ clinician who can help you, or your loved one, struggling with suicidal thoughts and feelings.