Suicide rates are on the rise. Saving lives takes a village.
CAMS is one effective treatment method for suicide-focused care. But we can’t do it alone. A comprehensive ecosystem of care that puts the individual suffering with suicidal thoughts and behaviors at the center is imperative.
CAMS integrates with comprehensive suicide prevention systems, from public and community awareness to evaluation of suicide risk and evidence-based treatments like DBT, and CT-SP.
Together, we can work together to minimize the number of patient touchpoints and provider time limitations to give the patient the best possible care.
Systems of Care Journey
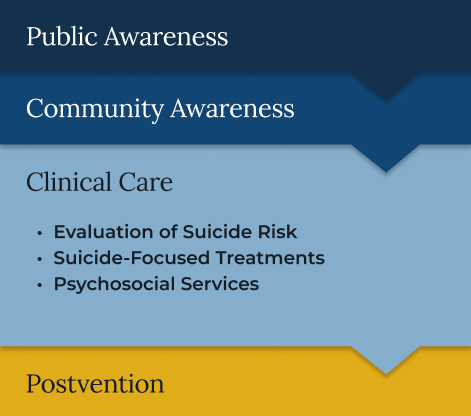
Providing the right resources for people experiencing suicidal thoughts and behaviors, ensuring they receive support without fear of invalidation or hospitalization.
Prepping the “gatekeeper”—the medical staff, school counselor, teacher, first responder, mental health professionals, or other, who listens and responds to someone expressing suicidal thoughts and behaviors—to respond appropriately.
Training tools like LivingWorks, QPR, CALM can educate these gatekeepers to better support those in need.
Equipping the provider to identify a person’s suicidal risk through a brief screening with well-established tools such as Ask Suicide-Screening Questions (ASQ) and the PHQ-9, as well as to conduct a therapeutic assessment and safeguarding plan using tools such as the Suicide Status Form, C-SSRS (Columbia-Suicide Severity Rating Scale), the Scale for Suicide Ideation (SSI), the Suicide Intent Scale (SIS), the Suicide Behaviors Questionnaire (SBQ), or other Suicide-Focused Treatments.
Treating suicidal risk through evidence-based frameworks, such as CAMS, DBT, CT-SP, and BCBT.
Evidence-Based treatment, such as CAMS, DBT, CT-SP, and BCBT are known to be the most effective methods.
Leveraging other efforts to reduce suicide attempts, such as Non-Demand Caring Contacts, or one-way, caring communication (letters, postcards, texts, emails, and phone calls).
There’s also personalized, self-care technological advances with platforms like NeuroFlow, bhworks, and WellTrack have high rates of engagement. Jaspr Health, a tablet and app for emergency department and post discharge use, empowers evidence-based suicide care at scale.
Supporting the patient after discharge through holistic case management to find jobs, housing, transportation, and around-the-clock support with services like Protocall to connect individuals with the help they need during crises.
The Zero-Suicide Framework
The Zero Suicide Initiative (Zero Suicide) aims to elevate suicide identification and care in healthcare systems.
Since its launch in 2012 and as part of the 2024 National Action Alliance for Suicide Prevention, Zero Suicide has shown notable reductions in suicide and suicide behaviors. It has also shown improvements to using evidence-based practices.
Zero Suicide promotes providers’ evidence-based practices by implementing the seven core elements below. CAMS specializes in training, identifying, engaging, and most importantly, treating.
