It was a hot summer afternoon half a dozen years ago and I was talking to a couple of new colleagues, Dr. Linda Dimeff and Kelly Koerner, both of whom had trained under and worked with my research mentor Marsha Linehan (the famous developer of Dialectical Behavior Therapy–DBT). Linda was describing to me a fascinating study that was conducted at the University of Boston using a computer-based avatar of a medical-surgical discharge nurse (named “Nurse Louise”). The clinical trial study that we were discussing compared the impact of the Nurse Louise avatar to a living discharge nurse in terms of patient compliance with discharge orders. To my amazement the outcomes for the avatar “nurse” were far superior to the living nurse with significant reductions in recidivism (among other desirable outcomes).
Linda then asked me about the general experience of suicidal patients in emergency departments (EDs), which I knew to be uniformly negative (both as a clinician and from the relevant ED/suicide literature). Linda then proposed something outlandish: that we go for a NIMH Small Business Innovation Research (SBIR) grant to create an all new avatar-based intervention using a modified version of CAMS as the heart of the assessment and intervention.

Ultimately this initial conversation led to a “proof of concept” Phase I NIMH SBIR grant that supported the creation and preliminary investigation of “Dr. Dave”—a rather pedestrian avatar based on me! The patient will work through a CAMS-based Suicide Status Interview (SSI) assessment for suicidal ED patients while they wait, often for many hours, to see their ED doctor for evaluation and treatment disposition.
The Phase I study was a resounding success and we published an initial paper of our findings in a peer-review journal. The success of this proof of concept lead to a Phase II SBIR grant from NIMH to conduct a randomized controlled trial (RCT) of this new ED-based intervention. I have come to truly love this line of research for many reasons.
Perhaps foremost in my mind, is that with some exceptions (for example, the inspired work by Dr. Ed Boudreaux), the ED has largely been completely ignored as a place to effectively work with suicidal risk. And yet every day around the world, suicidal people sit 6, 10, or 20 hours sometimes being “boarded” overnight waiting to see their ED doctor. For patients struggling with acute suicidal pain this ED wait is an intolerable eternity and it is not uncommon that patients simply give up and walk out the door.
Another amazing thing about this research has been the incredible engagement of people with lived experience (those individuals who have previously been suicidal, made attempts, and sat in ED for countless hours). We have harnessed the power of this perspective which has transformed the Dr. Dave avatar experience into “Jaspr Heath” which is now a multipurpose tablet-based engagement experience that still features the CAMS-based SSI assessment and a version of CAMS intervention in the form of a Stabilization Plan. Dr. Dave is gone and has been replaced by a virtual guide named “Jasper” (a little cartoon character) or a pleasant looking woman, by the name of “Jaz” (a much better alternative to my original avatar, which frankly, frightened my wife and kids).
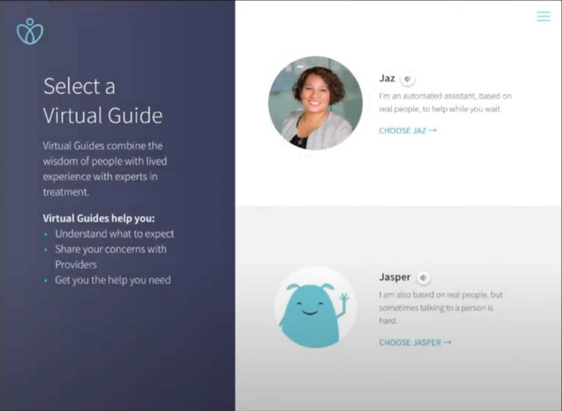
“Jasper” or “Jaz” can then introduce a full array of options to engage the suicidal ED patient, including education about the ED experience and what to expect while they are there. Patients are offered access to a menu of “Comfort and Skills” which is content to help them learn new options for coping, ranging from DBT-inspired coping skills to comforting video content of puppies playing, a crackling fireplace, to distracting techniques, etc. There is also an option to engage in video content of people with lived experience who provide hope and inspiration through their own stories of despair and redemption and lessons learned.
The Jaspr Health patient engagement ultimately produces a detailed report for busy ED providers that provides key assessment information about the patient’s suicidal risk, their CAMS-inspired Stabilization Plan, information about their access to lethal means (and willingness to secure such means), and further considerations that should help shape and inform an optimal disposition plan for the patient. For their engagement with Jaspr, patients are provided a digital companion app of their “favorite” content from the Jaspr engagement that they can download to their smart phone or laptop.
To get a taste of the Jaspr experience, check out a 2 minute YouTube video at: https://www.youtube.com/watch?v=l9zbM8jEsvY&feature=youtu.be)
As per Phase II, in the last year we began using Jaspr Health in a rigorous RCT within ED care at the famed Mayo Clinic in Rochester MN. It is fair to say, that doing ED-based research is challenging even in the best of circumstances. But adding the worldwide COVID-19 pandemic to the mix made our ED-based research impossible to further pursue and the RCT was abruptly interrupted in March to accommodate needed ED space and focus on COVID-19 patients. With about a third of the sample recruited, we went ahead and did a preliminary analysis of the 30+ ED patients that had been engaged in the RCT prior to COVID-19 preempting further RCT data collection. With limited statistical power (due to the small sample), we were nevertheless thrilled with significant and favorable findings fully supporting the use of Jaspr Health. I will leave the particulars for a later blog as the study and our preliminary results are now under review in a paper that we recently submitted to a peer-reviewed journal. But suffice it to say, even we were stunned by the incredibly positive results from suicidal ED patients’ engagement with Jaspr. We are planning to continue the Jaspr RCT when the COVID-19 transmission and infection rates become more stable.
The Jaspr research experience has been an unexpected gift within my professional life. I have never been particularly savvy with technology and as a provider and professor of clinical psychology, I am very biased to favor a live person-to-person clinical engagement between a provider and patient. But the Jaspr experience has taught me new lessons about what can work in the service of saving lives. The technology of Jaspr is impressive. The ED experience is uniformly negative, but the Jaspr engagement makes it much more tolerable and ensures that time in the ED a productive and valuable experience for the patient with benefits for busy ED providers as well.
These benefits of Jaspr need not end as the patient leaves the ED because they will have access to Jaspr-based content that is downloaded to their phone or laptop. I am a pragmatist, and with 10,600,000 adult Americans struggling with serious suicidal ideation each year, we need any and all help possible to address that suffering in the service of saving more lives from suicide. As our research continues to unfold, I am convinced that Jaspr can play a key role in that pursuit.
