Suicide claims one person in the U.S. every 12 minutes, according to the CDC. That’s 123 lives lost each day in America alone.
Many of these people reach out to or are referred to counseling or other treatment and interventions intended to prevent an eventual death by suicide, but unfortunately – and despite the best of intentions – most of these therapists and professionals are undertrained (or not trained at all) and ill-equipped to effectively help these troubled individuals.
Two major obstacles stand in the way of developing and delivering effective training for those in the suicide prevention and treatment field: insufficient funds availability and a lack of national standards.
Lack of Funding for Suicide Prevention and Treatment in General
As pointed out in a 2018 article by USAToday, although the CDC reports that suicide is the 10th leading cause of death in the United States, and the second leading cause of death in youth, funding for suicide prevention and treatment lags behind other top killers.
In fact, according to NIH, Centers for Disease Control and Prevention, more funds are available for vision disorders, intellectual and developmental disabilities, sleep research, and dietary supplements than for suicide prevention – all associated with conditions having much lower mortality rates than death by suicide.
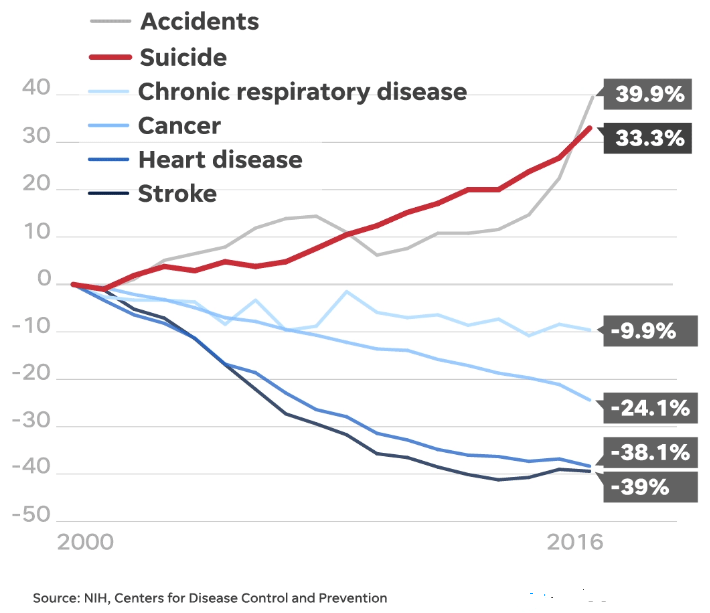
Additionally, with the exception of accidents, the same study shows that the leading causes of death have declined since 1999, while the suicide rate has increased by 33.3%.
Conducting research projects and completing randomized controlled trials (RCTs) needed to determine effective prevention and treatment methods can be expensive, and the costs of developing evidence-based and outcome-based programs and running treatment centers are prohibitive for many organizations.
With this lack of funds for suicide assessment and treatment in general, it follows that training in effective assessment and treatment is also lacking – and that is certainly distressing for those in this field.
No National Standards Requiring Training for Suicide Prevention and Treatment
As reported in the American Journal of Public Health, a study completed in 2017 found that only ten states currently mandate training for behavioral healthcare professionals in how to spot risk for suicide and take preventative action. Furthermore, there are no national standards requiring training. The study identified the following:
- # of states with policies mandating and encouraging suicide prevention training for healthcare professionals: 2
- # of states with a policy mandating suicide prevention education for healthcare professionals: 8
- # of states with a policy encouraging suicide prevention education for healthcare professionals: 5
- # of states with a policy mandating or encouraging training for the treatment for suicidal patients for healthcare professionals: 0
The same report, which emphasizes deficiencies in mental health training, asserts that accrediting organizations must include suicide-specific training and education in their graduate programs, and furthermore, the government should require such training for healthcare systems receiving state or federal funds.
The Dangers of These Obstacles
We all want to help, but the fear of doing or saying the wrong thing and failing to effectively treat a person in need can have devastating effects.
In fact, with no other option in sight, poorly trained therapists often resort to referring suicidal clients to the emergency room. However, studies show that emergency department presentation and admission into psychiatric hospitalization can actually increase the risk of a lethal outcome in people with suicidal ideation.
In addition to a fear of failing to successfully treat a suicidal client, there’s also the concern of exposure to malpractice liability and the risk of losing one’s license to practice. In their confusion and grief, families of suicide victims often look for external causes for the loss of their loved ones, sometimes landing on the actions or inactions of those who were meant to help.
Too often, these fears leave suicidal patients without the care, treatment, or interventions that they so desperately need.
Overcoming Obstacles to Training
If suicide were more commonly and widely viewed as a leading public health issue, as other leading risks are, perhaps more funds would be allocated to suicide prevention and treatment, and more focus would be put on developing standards for effective training.
In the meantime, CAMS-care offers training in the evidence-based and outcome-based Collaborative Assessment and Management of Suicidality (CAMS) Framework, developed by Dr. David A. Jobes over the course of the last 30 years.
With a robust base of clinical trial research, the CAMS Framework® presents a collaborative approach to suicide assessment, intervention, and treatment. Flexible and affordable training, available both online and onsite, helps healthcare providers and other individuals become more confident in their ability to help their clients and patients with suicidal ideation and risk and avoid lethal outcomes.
