Vermont’s suicide rate has increased by 73.1% since 1999, which marks the 4th largest increase of any state over this time period. Prior to 2008 there was no structured approach in Vermont for reducing suicide deaths in the State.
In 2008, a small group of suicide loss survivors, non-profit and state partners applied for and received a three-year Garrett Lee Smith (GLS) grant from the Substance Abuse and Mental Health Service Administration (“SAMSHA”) to promote suicide prevention among youth. A second GLS Grant was received in 2011, bolstering the emergence of a strong statewide cross-sector Coalition managed by the Center for Health and Learning. The Vermont Suicide Prevention Coalition committed themselves to a lifespan approach and developed the Vermont Suicide Prevention Platform-Working to Prevent Suicide Across the Lifespan. The Platform was based on the National Strategy for Suicide Prevention and has served as a guidance document for the state.
An infrastructure survey indicated the need for an entity to provide leadership and direction for suicide prevention, and the Vermont Suicide Prevention Center (VTSPC) was formed as a public-private partnership to provide sustainability beyond the federal grant, and to ensure input from PWLE and a multi-sector approach. The Center has sustained its work for the past five years on a small state allocation, coupled with projects funded by foundations, and private donor support.
In 2011, Dr. Jay Batra, the medical director of the state hospital system, and Dr. JoEllen Tarallo, the Executive Director for the Center for Health and Learning, and Director of the VTSP Center, attended the annual American Association of Suicidology conference where they listened to Dr. Michael Hogan’s presentation on the Zero Suicide Initiative: a system-wide organizational commitment to safer suicide care in health and behavioral health care systems. Zero Suicide is an approach that meets Goal #7 of the Vermont Platform: Promote suicide prevention, screening, intervention, and treatment as core components of health care services with effective clinical and professional practices.
The Zero Suicide Initiative includes a toolkit introducing the following seven elements:
| 1. | LEAD | System-wide culture change committed to reducing suicides |
| 2. | TRAIN | A competent, confident and caring workforce |
| 3. | IDENTIFY | Individuals with suicide risk via a comprehensive screening and assessment |
| 4. | ENGAGE | All individuals at-risk of suicide using a suicide care management plan |
| 5. | TREAT | Suicidal thoughts and behaviors using evidence-based treatments |
| 6. | TRANSITION | Individuals through care with warm hand-offs and supportive contacts |
| 7. | IMPROVE | Policies and procedures through continuous quality improvement |
Dr. Hogan’s presentation inspired Dr. Batra and Dr. Tarallo to create Vermont’s own Zero Suicide Initiative.
The Coalition has maintained a strong presence annually at the statehouse, and a one-time allocation of $50,000 has grown to an annual grant of $220,000 from the State to support a population-wide health approach to suicide prevention focused on reducing the number of Vermonters who die by suicide each year. The purpose(s) of the Program is to:
- Support public education and information to improve awareness and access to suicide prevention support and services;
- Develop and support policy, stakeholder engagement, and a suicide prevention infrastructure to improve suicide prevention planning and implementation;
- Advance best and evidence-based practices for suicide prevention through workforce development;
- Promote social and emotional wellness to prevent suicides in Vermont.
This is a lot of work to do with just $220,000 a year, and yet the Vermont Suicide Prevention Center has continued its work to comprehensively build a Zero Suicide system of care that addresses all the elements of the Zero Suicide Toolkit.
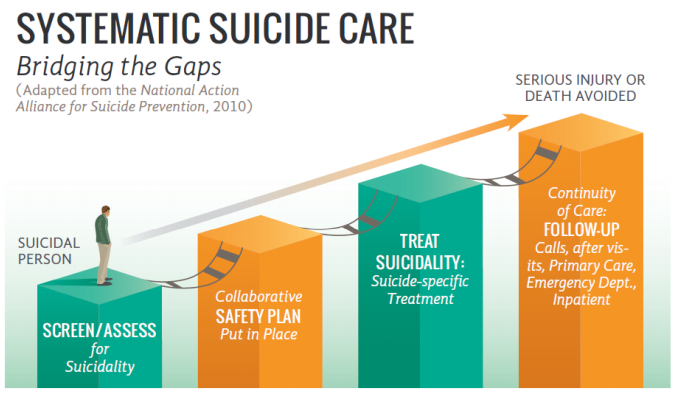
As this graphic illustrates, in Vermont’s continuum of care the staff use a number of tools to identify, engage, treat, and transition clients.
CAMS’ Role
Within the Vermont pathway to suicide safer care, Umatter, ASIST, and/or QPR are used to train the community and workforce as Gatekeepers, to recognize warning signs, know what to say and do, and how to get help. A standard screening and assessment form (the C-SSRS) is used to identify suicidal ideation, leading to the client being seen by a clinician trained to treat that person using the Collaborative Assessment and Management of Suicidality (CAMS).
The evidence base for CAMS made it an obvious choice to adopt as a treatment in Vermont’s system of care. Dr. Tarallo explained that “the state Zero Suicide Steering Group, which was composed of a variety of clinicians and stakeholders, selected CAMS because of the research base, its strong track record as both an assessment and treatment tool, and because it promotes a collaborative approach with the patient using a set of structured tools. The group was strongly influenced by the data which shows that a structured tool trumps individual professional discretion in a research-based trial every time. The body of evidence for CAMS and the Suicide Status Form is significant and robust.”
Measuring Success
With a background in systems change management, Dr. Tarallo and her team have been using the Concerns Based Adoption Model (CBAM) to guide the implementation of the Vermont Suicide Prevention model. Successfully implementing a new program involves more than providing staff with materials, resources, and training. An often-overlooked factor is the human element—the people actually doing the work. Each person responds to a new program with unique attitudes and beliefs, and each person will use a new program differently. VTSPC has a long term relationship partnering with an evaluator from the Larner College of Medicine at the University of Vermont to evaluate program implementation and collect client level outcome data.
VTSPC has worked with more than 250 clinicians across seven mental health agencies and while they are using the same tools there are differences in approaches and hence variations in outcomes. VTSPC is currently collecting two of the 12 measures for Zero Suicide: screening and safety planning. For screening, they are looking at how many screenings are being performed and in which locations. Not all clinicians are using qualified safety planning tools so the goal is to review these documents and produce guidelines for consistency and quality standards.
A key part of measuring the success of the program is to have documentation and results available in the various Electronic Medical Records. CAMS-care is working with several agencies in Vermont to allow clinicians and mental health centers to use electronic versions of the Suicide Status Form, which will facilitate better tracking of people treated for suicidal ideation and the outcomes. Under short-term COVID relief emergency funding, the VTSPC is working with the VT Department of Mental Health and VT Department of Health Care Access to engage primary care practices in the Vermont “Blueprint” in the pathway of care.
Future Plans
VTSPC has developed a Zero Suicide program that is a model for many other organizations and States. Most impressively, they have achieved this with limited State funding.
With additional funding, the VTSPC would deploy such resources to:
- Raise awareness of the Zero Suicide program;
- Reduce the stigma of seeking help for those in need;
- Further invest in people and facilities to identify and treat suicidal people;
- Continue to train clinicians in evidence-based protocols and tools;
- Measure results to show that the Zero Suicide initiative is benefiting Vermonters.