
Navigating suicidal thoughts can feel isolating. However, suicidal ideation is more common than many may realize. In 2023, a combined 16 million adults and adolescents in the U.S. had “serious thoughts of suicide.” [1] These numbers show a major challenge in suicide prevention. They highlight a strong need for mental health support aimed at suicidal thoughts. Over the years, clinical trial researchers have developed several evidence-based therapies that provide relief and healing for those struggling with suicide. Whether you’re seeking support for yourself or a loved one, it’s important to understand which therapeutic approaches are available and are the most helpful for recovery.
What Causes Suicidal Thoughts?
Suicidal thoughts, or suicidal ideation, can result from a number of causes. However, it ultimately stems from the specific struggles the individual is facing. Research has shown that relational, vocational, and self-oriented issues tend to be the most common root causes of suicidal ideation .[2] For example, a failed relationship or high stress at work could be a factor. Low self-esteem due to bullying could also be a factor. A person may face many struggles in life. These struggles can lead to negative thoughts and feelings of hopelessness. While mental health disorders and other risk factors can also play a role, it’s important that the deeper issues are addressed.
When talking about suicidal ideation, it’s also important to identify the two types: passive and active. Passive suicidal ideation is when a person has thoughts of suicide but is not actively making a plan to harm themselves. Active suicidal ideation is when the thoughts of suicide motivate a person to create a plan to carry it out in the nearterm future. Both types of suicidal ideation require some kind of intervention, though active ideation requires more immediate attention.
When to Seek Professional Help
If you find yourself thinking about suicide frequently and actively avoid the people, places, and hobbies you usually enjoy, you should reach out for help. Early intervention is key when dealing with suicidal thoughts. The earlier suicidal ideation is dealt with, the greater likelihood of healing and avoiding negative outcomes. Early intervention helps stop these thoughts from getting worse. It also helps the person build resilience. They can learn tools and coping skills to manage their negative thoughts. Evidence-based therapies are the best place to start.
For those who are dealing with active suicidal ideation (i.e. making a plan), immediate help is needed. The 988 Suicide & Crisis Lifeline is a free resource that is available 24/7 for those who are struggling. Don’t hesitate to reach out if you need someone to talk to.
What are Evidence-Based Therapies?
Evidence-based therapies are those that provide research-based support to those who are struggling with a specific issue, such as suicidal ideation. These have been tested through rigorous trials and case studies. Evidence-based therapies and treatments make sure people get care that has been well tested. This care is supported by large-scale research. It is better to see a professional who specializes in suicide-specific therapies. This is more effective than visiting a general doctor or therapist for mental health issues. This can greatly help those in need and give them the tools to move forward.
Types of Evidence-Based Therapies
- Collaborative Management and Assessment of Suicidality (CAMS)
CAMS is widely recognized as the most effective treatment for those dealing with suicidal ideation. It is referenced in the Zero Suicide Toolkit and 2024 National Suicide Prevention Strategy. CAMS approaches suicidal ideation by first identifying the drivers of suicide and creating a plan to manage these drivers, helping reduce the risk of suicidal behavior. CAMS also uses quantitative and qualitative risk assessment in every session, including self reflection and discussion of risk factors, as well as methods to help people create a life that’s worth living. - Cognitive Behavioral Therapy-Suicide Prevention (CT-SP)
CBT is a type of talk therapy that has been effective for those dealing with issues such as depression, anxiety, eating disorders, and more. CT-SP is an intervention that specifically tailored to addressing those who are experiencing suicidal ideation. It takes the approach of helping individuals respond to their automatic thoughts, breaking negative patterns and building new, positive ones. One specific strategy in this therapy is the “Hope Kit” or “Hope Box.” This is a physical or digital space. Here, a person keeps important photos, notes, and other items. These items inspire them to keep living. - Brief Cognitive Behavioral Therapy (BCBT) is another form of CBT that is completed in a limited number of sessions, typically four to eight. Individuals will learn about the “suicidal mode” as well as self-soothing techniques and problem solving. Similar to CBT-SP, individuals will develop a “Hope Kit” and work to build new, positive thought patterns. The final phase of care involves creating a relapse prevention protocol.
- Dialectical Behavior Therapy (DBT)
DBT helps people to embrace acceptance and learn coping strategies for times of dealing with distress. It is often used to treat those with borderline personality disorder (BPD), major depressive disorder, bipolar disorder, and those who are struggling with suicidal thoughts. Some goals of DBT include learning and developing emotional regulation, problem-solving skills, and distress tolerance.
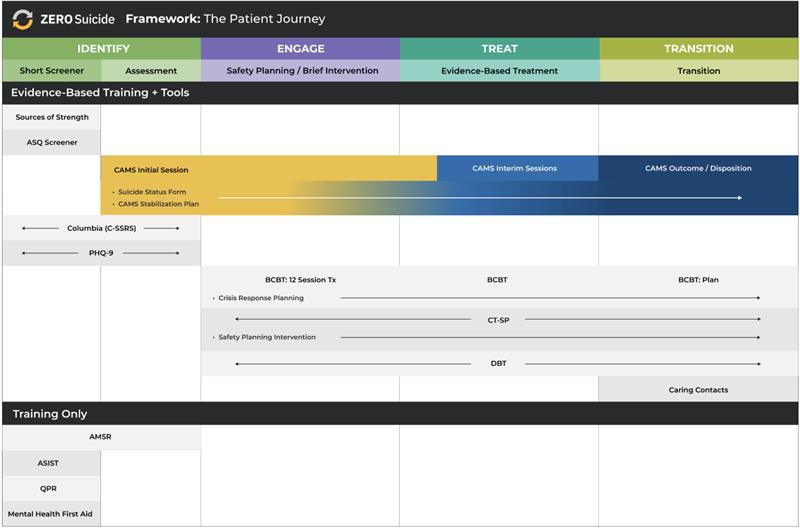
See a comparison of evidence-based therapies and screening/assessment tools.
Other Types of Support
In addition to therapy, there are other methods of support that can be helpful, including online resources that are available anytime. Now Matters Now offers videos and resources that teach coping strategies and skills. They also offer free, online peer support meetings where members can share their stories and practice skills together. The Lived Experience Academy is another online resource that offers support for healing, recovery, and growth after a crisis.
Hope is Always Here
Managing suicidal thoughts can feel overwhelming, but it’s important to remember that you are not alone. There are many effective options for different people and their unique situations. These include evidence-based therapies, mindfulness, and peer support. If you or someone you know is struggling, reach out for professional help. For immediate needs, contact the 988 Suicide & Crisis Lifeline for via text, online chat, or phone call.
Download the Patient Journey Comparison Chart